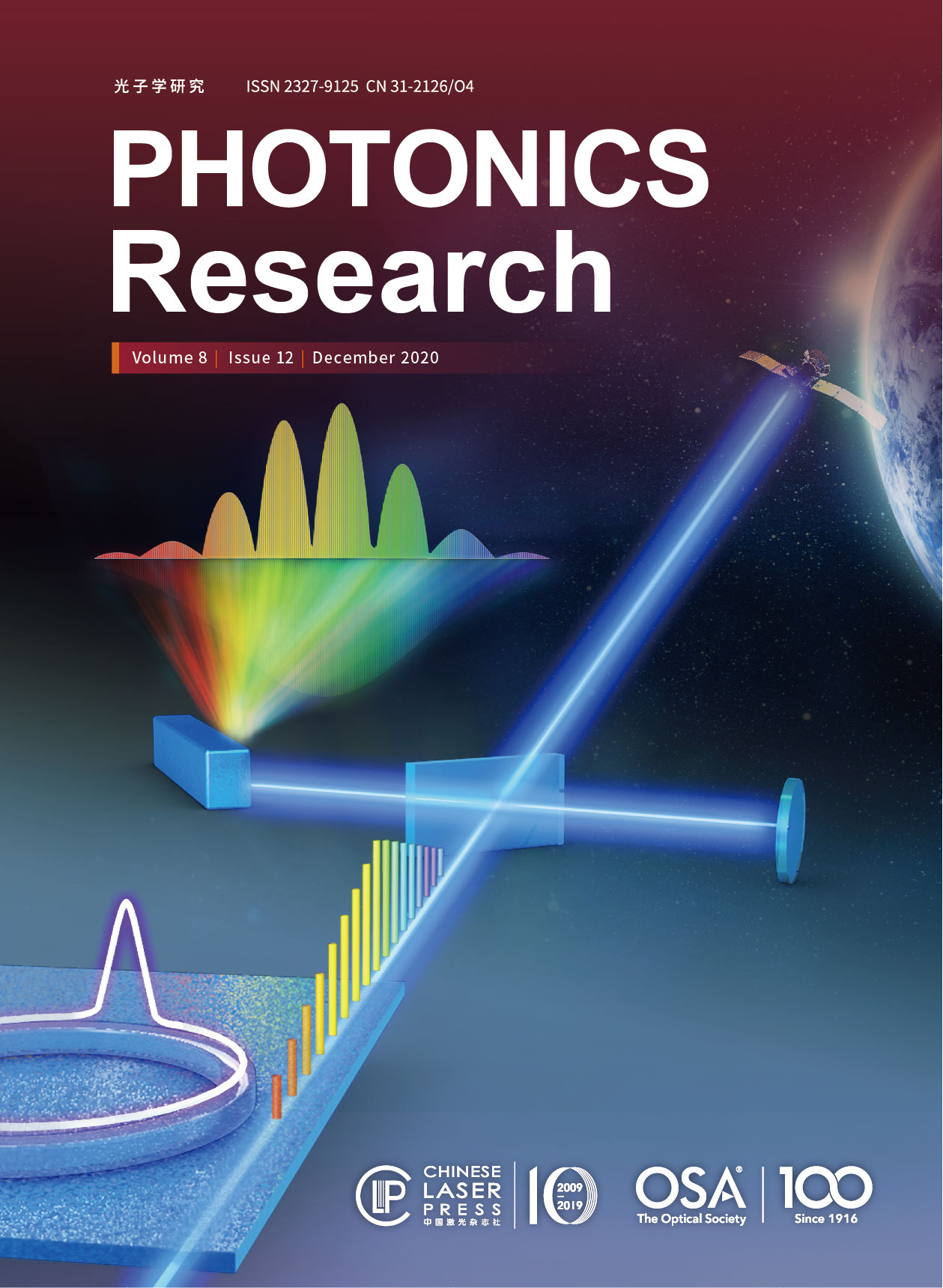
Confocal visible/NIR photoacoustic microscopy of tumors with structural, functional, and nanoprobe contrasts  Download: 720次
Download: 720次
Jiangbo Chen, Yachao Zhang, Xiaozhen Li, Jingyi Zhu, Dengfeng Li, Shengliang Li, Chun-Sing Lee, Lidai Wang. Confocal visible/NIR photoacoustic microscopy of tumors with structural, functional, and nanoprobe contrasts[J]. Photonics Research, 2020, 8(12): 12001875.
[8] S. Manohar, S. S. Gambhir. Clinical photoacoustic imaging. Photoacoustics, 2020, 19: 100196.
[39] J. Yao, L. V. Wang. Photoacoustic microscopy. Laser Photon. Rev., 2013, 7: 758-778.
[43] Y. Matsumura, H. Maeda. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res., 1986, 46: 6387-6392.
Jiangbo Chen, Yachao Zhang, Xiaozhen Li, Jingyi Zhu, Dengfeng Li, Shengliang Li, Chun-Sing Lee, Lidai Wang. Confocal visible/NIR photoacoustic microscopy of tumors with structural, functional, and nanoprobe contrasts[J]. Photonics Research, 2020, 8(12): 12001875.