[1] Miller P R, Aggarwal R, Doraiswamy A, et al. Laser micromachining for biomedical applications[J]. JOM, 2009, 61(9): 35-40.
[2] Ruddock I S, Bradley D J. Bandwidth-limited subpicosecond pulse generation in mode-locked cw dye lasers[J]. Applied Physics Letters, 1976, 29(5): 296-297.
[3] Fork R L, Greene B I, Shank C V. Generation of optical pulses shorter than 0.1 psec by colliding pulse mode locking[J]. Applied Physics Letters, 1981, 38(9): 671-672.
[4] Pronko PP,
VanRompay P A, Singh R K, et al. Laser induced avalanche ionization and electron-lattice heating of silicon with intense near IR femtosecond pulses[C]. MRS Proceedings,
1995,
397:
45-
51.
[5] LiX,
JiangL,
WangC,
et al. Transient localized material properties changes by ultrafast laser-pulse manipulation of electron dynamics in micro/nano manufacturing[J]. MRS Proceedings,
2011,
1365: mrss11-1365-tt01-01.
[6] Schaffer C B, Brodeur A, Mazur E. Laser-induced breakdown and damage in bulk transparent materials induced by tightly focused femtosecond laser pulses[J]. Measurement Science and Technology, 2001, 12(11): 1784-1794.
[7] Sanner N, Utéza O, Bussiere B, et al. Measurement of femtosecond laser-induced damage and ablation thresholds in dielectrics[J]. Applied Physics A, 2009, 94(4): 889-897.
[8] Le Harzic R, Huot N, Audouard E, et al. Comparison of heat-affected zones due to nanosecond and femtosecond laser pulses using transmission electronic microscopy[J]. Applied Physics Letters, 2002, 80(21): 3886-3888.
[9] Kautek W, Krüger J, Lenzner M, et al. Laser ablation of dielectrics with pulse durations between 20 fs and 3 ps[J]. Applied Physics Letters, 1996, 69(21): 3146-3148.
[10] Maselli V, Grenier J R, Ho S, et al. Femtosecond laser written optofluidic sensor: Bragg grating waveguide evanescent probing of microfluidic channel[J]. Optics Express, 2009, 17(14): 11719-11729.
[11] 成洁, 杨明红, 王闵, 等. 基于飞秒激光加工的马赫-曾德尔干涉氢气传感器[J]. 光学学报, 2012, 32(7): 0706001.
Cheng Jie, Yang Minghong, Wang Min, et al. Mach-Zehnder interference hydrogen sensor based on femtosecond laser processing[J]. Acta Optica Sinica, 2012, 32(7): 0706001.
[12] Gittard S D, Narayan R J. Laser direct writing of micro- and nano-scale medical devices[J]. Expert Review of Medical Devices, 2010, 7(3): 343-356.
[13] Nolte S, Chichkov B N, Welling H, et al. Nanostructuring with spatially localized femtosecond laser pulses[J]. Optics Letters, 1999, 24(13): 914-916.
[14] Liu Y, Sun S, Singha S, et al. 3D femtosecond laser patterning of collagen for directed cell attachment[J]. Biomaterials, 2005, 26(22): 4597-4605.
[15] Maruo S, Ikuta K, Korogi H. Submicron manipulation tools driven by light in a liquid[J]. Applied Physics Letters, 2003, 82(1): 133-135.
[16] Doraiswamy A, Jin C, Narayan R J, et al. Two photon induced polymerization of organic-inorganic hybrid biomaterials for microstructured medical devices[J]. Acta Biomaterialia, 2006, 2(3): 267-275.
[17] OstendorfA,
BauerT,
KorteF, et al.
Development of an industrial femtosecond laser micromachining system[C]. SPIE,
2002,
4633:
128-
135.
[18] 王桂森, 万熠, 王滕, 等. 植入体微纳结构表面制备及生物相容性研究综述[J]. 表面技术, 2016, 45(5): 8-18.
Wang Guisen, Wan Yi, Wang Teng, et al. Review on preparation of micro-nano structure on implant surface and its biocompatibility[J]. Surface Technology, 2016, 45(5): 8-18.
[19] Alves N M, Pashkuleva I, Reis R L, et al. Controlling cell behavior through the design of polymer surfaces[J]. Small, 2010, 6(20): 2208-2220.
[20] Seo C H, Jeong H, Furukawa K S. et al. The switching of focal adhesion maturation sites and actin filament activation for MSCs by topography of well-defined micropatterned surfaces[J]. Biomaterials, 2013, 34(7): 1764-1771.
[21] Anselme K, Bigerelle M. On the relation between surface roughness of metallic substrates and adhesion of human primary bone cells[J]. Scanning, 2014, 36(1): 11-20.
[22] Aebli N, Krebs J, Stich H, et al. In vivo comparison of the osseointegration of vacuum plasma sprayed titanium- and hydroxyapatite-coated implants[J]. Journal of Biomedical Materials Research Part A, 2003, 66A(2): 356-363.
[23] Dumas V, Rattner A, Vico L. et al. Multiscale grooved titanium processed with femtosecond laser influences mesenchymal stem cell morphology, adhesion, and matrix organization[J]. Journal of Biomedical Materials Research Part A, 2012, 100A(11): 3108-3116.
[24] Cunha A, Serro A P, Oliveira V. et al. Wetting behaviour of femtosecond laser textured Ti-6Al-4V surfaces[J]. Applied Surface Science, 2013, 265: 688-696.
[25] Oliveira V, Polushkin N I, Conde O, et al. Laser surface patterning using a Michelson interferometer and femtosecond laser radiation[J]. Optics & Laser Technology, 2012, 44(7): 2072-2075.
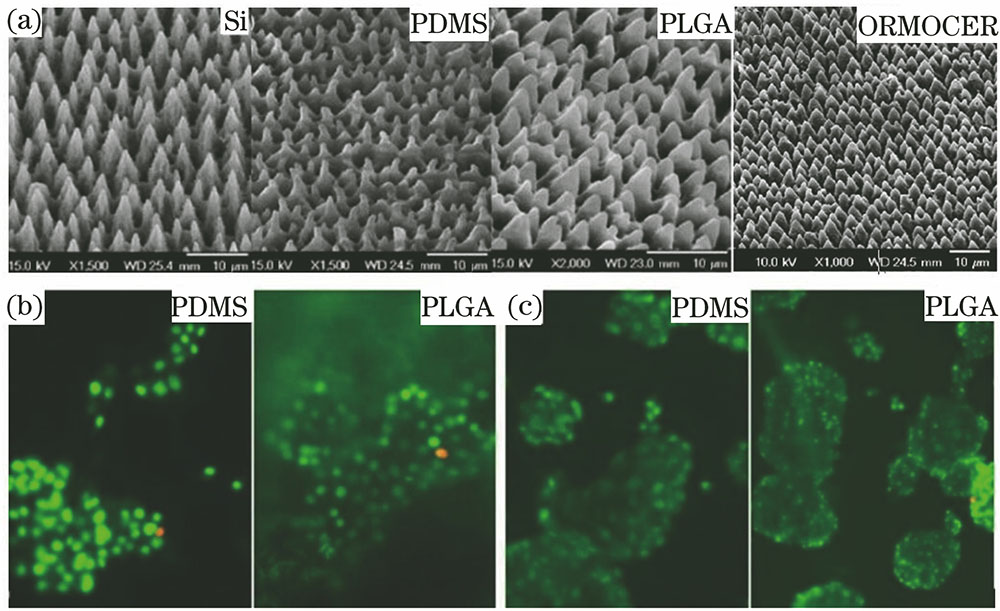
[26] Koufaki N, Ranella A, Aifantis K E, et al. Controlling cell adhesion via replication of laser micro/nano- textured surfaces on polymers[J]. Biofabrication, 2011, 3(4): 045004.
[27] 王瑞, 周延民. 飞秒激光在钛合金表面改性中的应用及其对成骨细胞黏附和增殖的影响[J]. 吉林大学学报(医学版), 2013, 39(3): 453-457.
Wang Rui, Zhou Yanmin. Application of femto-second laser in titanium alloy surface modification and its influence in adhesion and proliferation of osteoblasts[J]. Journal of Jilin University (Medicine Edition), 2013, 39(3): 453-457.
[28] Dumas V, Guignandon A, Vico L, et al. Femtosecond laser nano/micro patterning of titanium influences mesenchymal stem cell adhesion and commitment[J]. Biomedical Materials, 2015, 10(5): 055002.
[29] Cunha A, Zouani O F, Plawinski L, et al. Human mesenchymal stem cell behavior on femtosecond laser-textured Ti-6Al-4V surfaces[J]. Nanomedicine, 2015, 10(5): 725-739.
[30] Zhang R, Wan Y, Ai X, et al. Preparation of micro-nanostructure on titanium implants and its bioactivity[J]. Transactions of Nonferrous Metals Society of China, 2016, 26(4): 1019-1024.
[31] Allegrini Jr S, Yoshimoto M, Barbosa Salles M, et al. Biologic response to titanium implants with laser-treated surfaces[J]. International Journal of Oral & Maxillofacial Implants, 2014, 29(1): 1-8.
[32] Sa A R, Mousavi S A, Seyedjafari E, et al. Polycarbonate surface cell's adhesion examination after Nd∶YAG laser irradiation[J]. Materials Science and Engineering C, 2009, 29(4): 1491-1497.
[33] Spearing S M. Materials issues in microelectromechanical systems (MEMS)[J]. Acta Materialia, 2000, 48(1): 179-196.
[34] Birmpiliotis D, Czarnecki P, Koutsoureli M, et al. Assessment of dielectric charging in capacitive MEMS switches fabricated on Si substrate with thin oxide film[J]. Microelectronic Engineering, 2016, 159: 209-214.
[35] JeongJ,
ShinS,
Lee GJ,
et al. Advancements in fabrication process of microelectrode array for a retinal prosthesis using liquid crystal polymer (LCP)[C]. IEEE,
2013:
5295-
5298.
[36] Green R A, Ordonez J S, Schuettler M, et al. Cytotoxicity of implantable microelectrode arrays produced by laser micromachining[J]. Biomaterials, 2010, 31(5): 886-893.
[37] Suaning GJ,
SchuettlerM,
Ordonez JS,
et al. Fabrication of multi-layer, high-density micro-electrode arrays for neural stimulation and bio-signal recording[C]. CNE '07. 3rd International IEEE/EMBS Conference on Neural Engineering,
2007:
5-
8.
[38] Safadi MR,
Scott AJ,
ThakurJ, et al.
Fabrication of a waveguide for biomedical applications using novel micromachining techniques[C]. SPIE,
2004,
5588:
205-
213.
[39] Yuan D, Das S. Experimental and theoretical analysis of direct-write laser micromachining of polymethyl methacrylate by CO2 laser ablation[J]. Journal of Applied Physics, 2007, 101(2): 024901.
[40] Teixidor D, Orozco F, Thepsonthi T, et al. Effect of process parameters in nanosecond pulsed laser micromachining of PMMA-based microchannels at near-infrared and ultraviolet wavelengths[J]. The International Journal of Advanced Manufacturing Technology, 2013, 67(5-8): 1651-1664.
[41] Criales L E, Orozco P F, Medrano A, et al. Effect of fluence and pulse overlapping on fabrication of microchannels in PMMA/PDMS via UV laser micromachining: modeling and experimentation[J]. Materials and Manufacturing Processes, 2015, 30: 890-901.
[42] GuoX,
TavakoliB,
Kang HJ, et al.
Photoacoustic active ultrasound element for catheter tracking[C]. SPIE ,
2014,
8943:
89435M.
[43] Bell J A, Saikus C E, Ratnayaka K, et al. A deflectable guiding catheter for real-time MRI-guided interventions[J]. Journal of Magnetic Resonance Imaging, 2012, 35(4): 908-915.
[44] Lee K K C, Munce N R, Shoa T, et al. . Fabrication and characterization of laser-micromachined polypyrrole-based artificial muscle actuated catheters[J]. Sensors and Actuators A: Physical, 2009, 153(2): 230-236.
[45] WongwiwatP,
Narayan RJ,
Lee Y S. Improving biocompatibily of laser micromachined silicon wafer by surface cating with poly (
ethyleneglycol)
diacrylate and
diamond-like carbon for biomedical devices[C]. ASME,
2010,
MSEC2010-34283:
273-
280.
[46] Crucho C I C, Barros M T. Formulation of functionalized PLGA polymeric nanoparticles for targeted drug delivery[J]. Polymer, 2015, 68: 41-46.
[47] Zehbe R, Zehbe K. Strontium doped poly-ε-caprolactone composite scaffolds made by reactive foaming[J]. Materials Science and Engineering: C, 2016, 67: 259-266.
[48] Kim M S, Son J G, Lee H J, et al. Highly porous 3D nanofibrous scaffolds processed with an electrospinning/laser process[J]. Current Applied Physics, 2014, 14(1): 1-7.
[49] Wang J, Valmikinathan C M, Liu W, et al. Spiral-structured,nanofibrous, 3D scaffolds for bone tissue engineering[J]. Journal of Biomedical Materials Research Part A, 2010, 93(2): 753-762.
[50] Kancharla V V, Chen S. Fabrication of biodegradable polymeric micro-devices using laser micromachining[J]. Biomedical Microdevices, 2002, 4(2): 105-109.
[51] 钟敏霖, 范培迅. 激光纳米制造技术的应用[J]. 中国激光, 2011, 38(6): 0601001.
Zhong Minlin, Fan Peixun. Applications of laser nano manufacturing technologies[J]. Chinese J Lasers, 2011, 38(6): 0601001.
[52] Meng H, Liao J, Zhou Y, et al. Laser micro-processing of cardiovascular stent with fiber laser cutting system[J]. Optics & Laser Technology, 2009, 41(3): 300-302.
[53] Muhammad N, Whitehead D, Boor A. et al. Comparison of dry and wet fibre laser profile cutting of thin 316L stainless steel tubes for medical device applications[J]. Journal of Materials Processing Technology, 2010, 210(15): 2261-2267.
[54] HendricksF,
PatelR,
Matylitsky VV.
Micromachining of bio-absorbable stents with ultra-short pulse lasers[C]. SPIE,
2015,
9355:
935502.
[55] Kathuria Y P. Laser microprocessing of metallic stent for medical therapy[J]. Journal of Materials Processing Technology, 2005, 170(3): 545-550.
[56] 黄远, 田筝, 刘文西, 等. 加工工艺对医用心血管支架生物相容性的影响[J]. 天津大学学报(自然科学与工程技术版), 2003, 36(3): 374-379.
Huang Yuan, Tian Zheng, Liu Wenxi, et al. Influence of process techniques on biocompatibility of coronary artery stent[J]. Journal of Tianjin University (Sci Technol), 2003, 36(3): 374-379.
[57] Zeng R, Dietzel W, Witte F. et al. Progress and challenge for magnesium alloys as biomaterials[J]. Advanced Engineering Materials, 2008, 10(8): B3-B14.
[58] Farè S, Ge Q, Vedani M. et al. Evaluation of material properties and design requirements for biodegradable magnesium stents[J]. Matéria, 2010, 15(2): 96-103.
[59] Demir AG,
PrevitaliB,
ColomboD, et al.
Fiber laser micromachining of magnesium alloy tubes for biocompatible and biodegradable cardiovascular stents[C]. SPIE,
2012,
8237:
823730.
[60] 张亚臣, 荣烨之. 医用聚乳酸的生物特性及其临床应用[J]. 上海医学, 2005, 28(1): 79-80.
[61] StolbergK,
FriedelS,
KremserB, et al.
IR and green femtosecond laser machining of heat sensitive materials for medical devices at micrometer scale[C]. SPIE,
2014,
8968:
89680E.
[62] 程萍, 位迪, 吴本科, 等. 可降解心脏支架的飞秒激光精密加工[J]. 光学精密工程, 2014, 22(1): 63-68.
Cheng Ping, Wei Di, Wu Benke, et al. Femtosecond laser precision machining of biodegradable heart stent[J]. Optics and Precision Engineering, 2014, 22(1): 63-68.
[63] Langer R, Vacanti J P. Tissue engineering[J]. Science, 1993, 260(5110): 920-926.
[64] Prabhakaran M P, Venugopal J, Kai D, et al. Biomimetic material strategies for cardiac tissue engineering[J]. Materials Science and Engineering: C, 2011, 31(3): 503-513.
[65] Chiu Y W, Chen W P, Su C C, et al. The arrhythmogenic effect of self-assembling nanopeptide hydrogel scaffolds on neonatal mouse cardiomyocytes[J]. Nanomedicine: Nanotechnology, Biology and Medicine, 2014, 10(5): 1065-1073.
[66] Saranya N, Saravanan S, Moorthi A, et al. Enhanced osteoblast adhesion on polymeric nano-scaffolds for bone tissue engineering[J]. Journal of Biomedical Nanotechnology, 2011, 7(2): 238-244.
[67] Heinemann S, Heinemann C, Jager M, et al. Effect of silica and hydroxyapatite mineralization on the mechanical properties and the biocompatibility of nanocomposite collagen scaffolds[J]. ACS Applied Materials & Interfaces, 2011, 3(11): 4323-4331.
[68] Anastasiou A D, Thomson C L, Hussain S A. et al. Sintering of calcium phosphates with a femtosecond pulsed laser for hard tissue engineering[J]. Materials & Design, 2016, 101: 346-354.
[69] Landers R, Hubner U, Schmelzeisen R, et al. Rapid prototyping of scaffolds derived from thermoreversible hydrogels and tailored for applications in tissue engineering[J]. Biomaterials, 2002, 23(23): 4437-4447.
[70] Wiria F E, Chua C K, Leong K F, et al. Improved biocomposite development of poly (vinyl alcohol) and hydroxyapatite for tissue engineering scaffold fabrication using selective laser sintering[J]. Journal of Materials Science: Materials in Medicine, 2008, 19(3): 989-996.
[71] Kolan K C R, Leu M C, Hilmas G E, et al. . Effect of material, process parameters, and simulated body fluids on mechanical properties of 13-93 bioactive glass porous constructs made by selective laser sintering[J]. Journal of the Mechanical Behavior of Biomedical Materials, 2012, 13: 14-24.
[72] Sobral J M, Caridade S G, Sousa R A, et al. Three-dimensional plotted scaffolds with controlled pore size gradients: effect of scaffold geometry on mechanical performance and cell seeding efficiency[J]. Acta Biomaterialia, 2011, 7(3): 1009-1018.
[73] Van Bael S, Chai Y C, Truscello S, et al. The effect of pore geometry on the in vitro biological behavior of human periosteum-derived cells seeded on selective laser-melted Ti6Al4V bone scaffolds[J]. Acta Biomaterialia, 2012, 8(7): 2824-2834.
[74] Chu T M G. In vivo evaluation of 13-93 bioactive glass scaffolds made by selective laser sintering (SLS)[J]. Biomaterials Science: Processing, Properties and Applications II: Ceramic Transactions, 2012, 237: 91-99.
[75] Fukuda A, Takemoto M, Saito T, et al. Osteoinduction of porous Ti implants with a channel structure fabricated by selective laser melting[J]. Acta Biomaterialia, 2011, 7(5): 2327-2336.
[76] 李祥, 李涤尘, 王林, 等. 基于RP的骨组织工程支架构造及生物学特性分析[J]. 中国机械工程, 2005, 16(12): 1117-1120.
Li Xiang, Li Dichen, Wang Lin, et al. Fabrication of bone tissue engineering scaffolds based on RP and analysis of biological properties[J]. China Mechanical Engineering, 2005, 16(12): 1117-1120.
[77] Huang W, Feng P, Gao C, et al. Microstructure, mechanical, and biological properties of porous poly (vinylidene fluoride) scaffolds fabricated by selective laser sintering[J]. International Journal of Polymer Science, 2015, 2015: 132965.
[78] Shuai C, Feng P, Zhang L, et al. Correlation between properties and microstructure of laser sintered porous β-tricalcium phosphate bone scaffolds[J]. Science and Technology of Advanced Materials, 2016, 14(5): 055002.
[79] Van Bael S, Chai Y C, Truscello S, et al. The effect of pore geometry on the in vitro biological behavior of human periosteum-derived cells seeded on selective laser-melted Ti6Al4V bone scaffolds[J]. Acta Biomaterialia, 2012, 8(7): 2824-2834.
[80] Leong K F, Cheah C M, Chua C K. Solid freeform fabrication of three-dimensional scaffolds for engineering replacement tissues and organs[J]. Biomaterials, 2003, 24(13): 2363-2378.
 下载: 2433次
下载: 2433次