肺动脉栓塞检测的可视中国人蒙特卡罗模拟分析  下载: 609次
下载: 609次
Pulmonary embolism (PE) is a clinical and pathophysiological syndrome in which an endogenous or exogenous embolus occludes the pulmonary artery or its branches, causing pulmonary circulatory impairment that can lead to severe pulmonary infarction, usually accompanied by cardiovascular disease. Currently, the most accurate method for detecting PE is digital subtraction angiography (DSA) of the pulmonary arteries. However, this detection method is invasive and can easily damage blood vessels or surrounding tissues and often causes additional complications. Therefore, non-invasive, real-time, and accurate detection of pulmonary artery hemodynamics is highly desirable. Near-infrared spectroscopy (NIRS) is a simple, rapid, portable, and relatively inexpensive technique for non-invasive deep-tissue hemodynamic monitoring, which is based on the spectral characteristics of oxyhemoglobin (HbO2) and deoxyhemoglobin (Hb), which are characteristics used to quantify tissue hemoglobin oxygen saturation for disease measurement. In recent years, an increasing number of research groups have chosen to use NIRS to monitor human diseases, and it has been validated for use in studies involving many tissue sites in the body. However, the study of photons in the human pulmonary artery site has not been conducted in depth. Therefore, the feasibility of using NIRS to detect pulmonary artery embolism is investigated in this study.
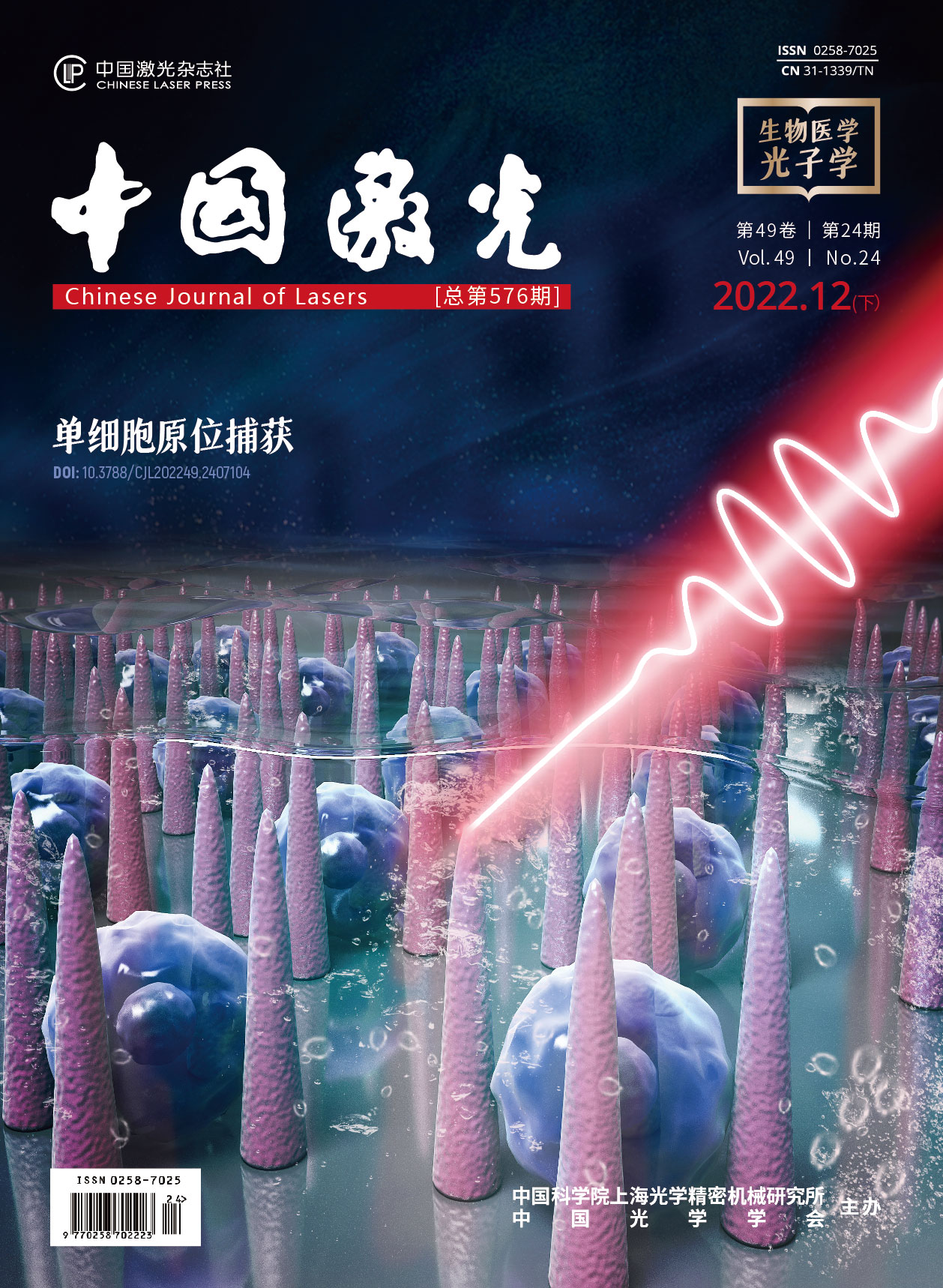
In this study, we used 80 photographic images from the Visual Chinese Human (VCH) dataset slices to map the thoracic tissue region of the pulmonary artery from top to bottom to build a 436×420×80 voxel thoracic photographic model (Figure 1). Each voxel is defined as a 0.4 mm×0.4 mm×0.4 mm cube. The entire model is divided into eight parts based on tissue type, including skin, muscle, bone, subcutaneous fat, lung, pulmonary artery, arterial blood, and venous blood. The constructed model is then loaded into a software program developed by our team for Monte Carlo simulation of light propagation in Voxelated Media (MCVM). MCVM generates two files: a photon absorption data file and a photon escape data file at the body surface, from which we can calculate a series of evaluation metrics to better evaluate the relationship between photon propagation and the separation of the light source and detector (LSD) in the VCH chest model.
According to photon absorption data, photons pass successively through the skin, fat, muscle, adipose tissue, and pulmonary artery to the venous blood. The intensity when reaching the pulmonary artery is estimated to be 45 voxel (Figure 3), which is sufficient to demonstrate that photons can cross the thoracic cavity and penetrate the experimental region of interest. Four indicators are introduced to study the optimized light source and detector distance: differential optical path-length factor (DPF), partial path-length factor (PPF), the ratio of PPF to DPF, and the proportion of photon absorption in the pulmonary artery. DPF increases exponentially with the increase of LSD,whereas the three other indicators (PPF, the ratio of PPF to DPF, and proportion of photo absorption in the pulmonary artery) trend upward and then downward, with the peak occurring in the 2.8-3.1 cm LSD range (Figure 4). Based on the above results, we selected 2.9 cm to study the effects of different degrees of pulmonary embolism on SSD (Table 3) and on the intensity of light detected on the body surface (Figure 5). As pulmonary embolism progressively worsens, the percentage of SSD present in the pulmonary arteries decreases (0.0131%, 0.0129%, 0.0127%, and 0.0126% in healthy, Level Ⅰ, Level Ⅱ, and Level Ⅲ subjects, respectively). The SSD proportions in arteriovenous blood and lungs were then evaluated for different degrees of pulmonary embolism. The results indicate that the proportion of SSD in the lung and venous blood gradually decreases as the degree of pulmonary embolism increases. However, the proportion of SSD in the arterial blood is almost zero. These results suggest that venous blood and lung tissue influence the sensitivity of the total assay. A one-dimensional linear regression analysis was performed by standardizing the light intensity of the measurement in the normal state and different embolic levels as independent variables. The results indicate that the standardized light intensity decreases with increasing levels of pulmonary embolism. Thus, the level of pulmonary embolism can be approximated using the detected light intensity.
This study implements noninvasive optical monitoring of pulmonary artery embolism based on the Visible Chinese Human dataset and use of Monte Carlo simulations. By simulating light migration in human thoracic tissues, the number of absorbed photons and the light fluence distribution in the thoracic tissues are derived, and the evidence suggests that some of the photons can reach the pulmonary artery, indicating that the proposed technique is feasible. In addition, this study proposes an optimized separation distance between the light source and the detector and concludes that a separation of 2.8-3.1 cm may be optimal based on two path length factors, PPF and DPF. The effect of pulmonary artery embolism on photon detection is verified based on SSD estimates at the pulmonary artery and the output photon intensity. The results indicate that the SSD at the pulmonary artery decreases with increasing embolization. Furthermore, light intensity directly correlates with the degree of embolization, and the presence of embolization can significantly decrease the light intensity, therefore indicating the presence of emboli in the pulmonary artery. Overall, this study demonstrates the great potential of NIRS for continuous bedside monitoring of pulmonary embolism.
王敏, 孟硕, 郭江辉, 李婷. 肺动脉栓塞检测的可视中国人蒙特卡罗模拟分析[J]. 中国激光, 2022, 49(24): 2407103. Min Wang, Shuo Meng, Jianghui Guo, Ting Li. Visible Chinese Human for Pulmonary Embolism Detection of Monte Carlo Simulation Analysis[J]. Chinese Journal of Lasers, 2022, 49(24): 2407103.